You are here
Inclusion of the optic nerve in the diagnostic criteria improves the detection of multiple sclerosis cases

The research findings propose to modify the McDonald 2017 criteria. However, they emphasize that it is not necessary to assess the presence of optic nerve lesions in all patients, only in those in whom diagnosis using the current criteria is not possible.
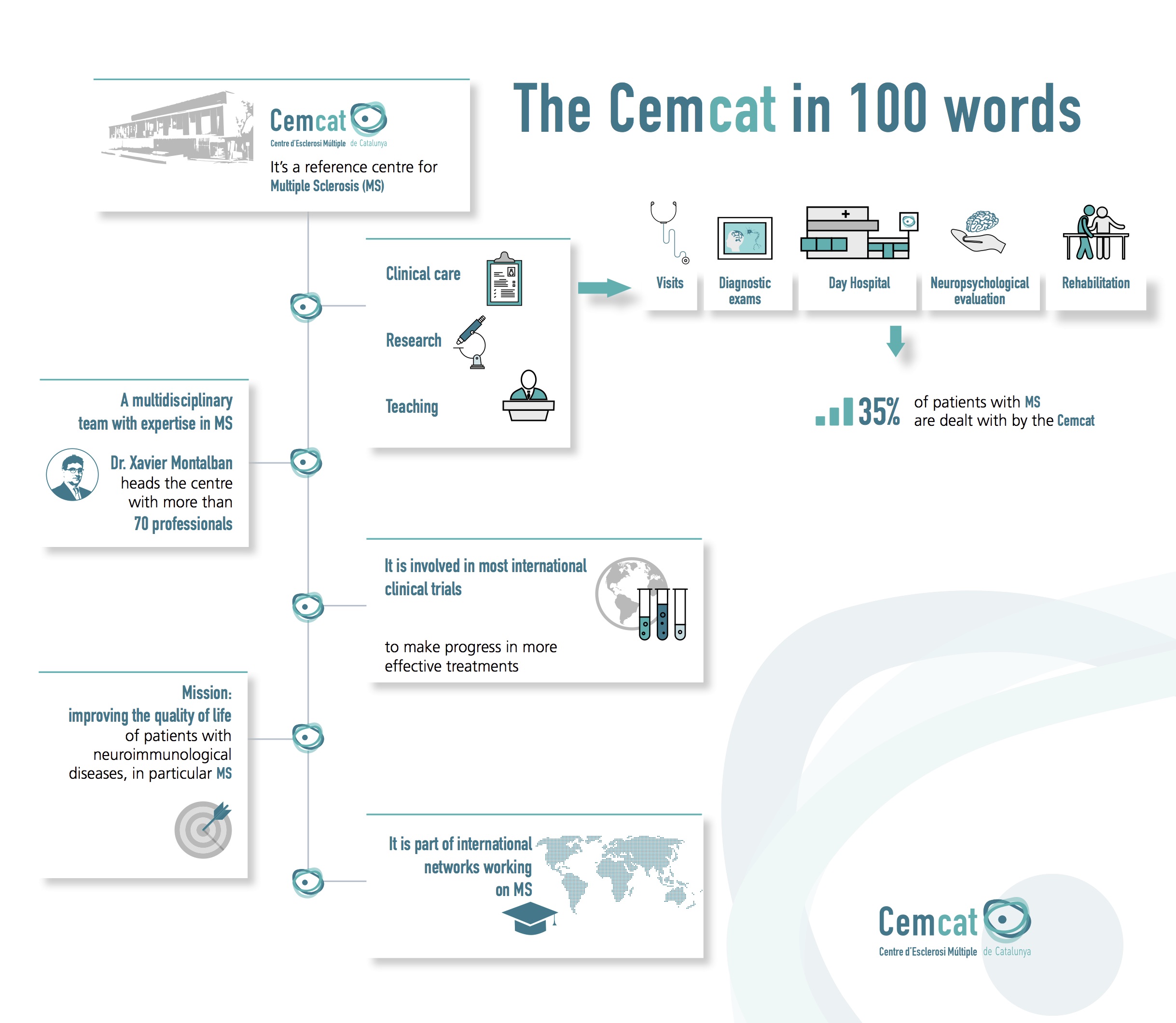
The multicenter study, coordinated by Dr. Xavier Montalban, director of the Multiple Sclerosis Center of Catalonia (Cemcat), the Neurology Service of the Vall d'Hebron University Hospital and the Clinical Neuroimmunology research group of the Vall d'Hebron Research Institute (VHIR), shows that the incorporation of the optic nerve into the diagnostic criteria would improve the ability to detect cases of multiple sclerosis.
"Inflammation of the optic nerve, or optic neuritis, is one of the most common manifestations of multiple sclerosis. In fact, one third of patients present it as the first symptom and seven out of ten develop it during the course of the disease," explains Dr. Angela Vidal Jordana, research neurologist at Cemcat, principal investigator of the Clinical Neuroimmunology group at VHIR and first author of the paper published in the journal Neurology. "However, nowadays, lesions in the optic nerve are not considered within the diagnostic criteria."
To diagnose multiple sclerosis, the McDonald criteria state that it is necessary to demonstrate spatial dissemination of demyelinating lesions. That is, involvement of at least two of four certain regions of the brain and spinal cord at different times. "The last revision of the McDonald criteria took place in 2017. Then, the optic nerve was not included as one of the regions of the central nervous system to be considered to confirm dissemination in space, due to a lack of data on its diagnostic utility. Consequently, when a patient arrives at the clinic with optic neuritis, but only one of the areas included in the criteria is affected, diagnosis and treatment are delayed until the appearance of a lesion in a second region," says Vidal Jordana.
The study involved 157 patients from 5 centers in the European Magnetic Resonance Imaging for Multiple Sclerosis (MAGNIMS) network. "The aim of our work was, on the one hand, to determine the impact of including optic nerve lesions in the diagnostic criteria. On the other, we sought to evaluate the ability of three tests, optic nerve MRI, optical coherence tomography and visual evoked potentials, to detect these damages," states Vidal Jordana. Data on optic nerve function were collected within six months of disease onset, using at least two of the three techniques.
According to the results, the inclusion of the optic nerve as a fifth study area improves sensitivity and diagnostic performance compared to the McDonald 2017 criteria. "We are talking about 92.5% sensitivity of the modified criteria versus 88.2% of the current criteria," specifies Montalban. "The strength of our proposal is that it does not change the minimum number of regions affected by concluding the diagnosis of multiple sclerosis. The McDonald criteria require lesions in two out of four regions. We maintain this two-region condition, but add a fifth area, the optic nerve, for those cases that do not quite meet the classic criteria. In other words, if magnetic resonance imaging already allows us to establish a clear diagnosis, it is not necessary to assess the function of the optic nerve".
Finally, the researchers emphasize that the modified criteria are applicable to any center that has one of the three techniques used in the study to evaluate the optic nerve, as they have similar performance.
Artículo de referencia
Angela Vidal-Jordana; Alex Rovira; Willem Calderon; Georgina Arrambide; Joaquín Castilló; Dulce Moncho; Kimia Rahnama; Sara Collorone; Ahmed T. Toosy; Olga Ciccarelli; Athina Papadopoulou; Nuria Cerdá-Fuertes; Johanna Lieb; Serena Ruggieri; Carla Tortorella; Claudio Gasperini; Alvino Bisecco; Rocco Capuano; Antonio Gallo; Andrea Barros; Annalaura Salerno; Cristina Auger; Jaume Sastre-Garriga; Mar Tintore; Xavier Montalban. Adding the optic nerve in multiple sclerosis diagnostic criteria: a longitudinal, prospective, multicenter study. Neurology. January 9, 2024 issue 102 (1) https://doi.org/10.1212/WNL.0000000000207805